 Weight Management is not about calories in and calories out. It can be far more complicated. Two hormones that play a crucial role in controlling when we eat but also when we don't are Ghrelin and Leptin. Working together they tell us when we're hungry and when we're not. Each are controlled by a variety of physical and psychological factors. German researchers have suggested that ghrelin levels play a big role in determining how quickly hunger comes back after we eat. Normally, ghrelin levels go up dramatically before you eat; this signals hunger. They then go down for about three hours after the meal. But some researchers believe that ghrelin is not as important in determining appetite as once thought. They think that its role in regulating body weight may actually be a more complex process. What We Know About Leptin -- the appetite suppressor -- appears to be the bigger player in our bodies' energy balance. Some researchers think that leptin helps regulate ghrelin. Leptin helps signal the brain that the body has enough energy stores such as body fat. But many obese people don't respond to leptin's signals even though they have higher levels of leptin. In general, the more fat you have, the more leptin is in your blood. But the level varies depending on many factors, including when you last ate and your sleep patterns. A study showed that rats that were given doses of leptin ended up eating less, but this effect lasted only about two weeks. It seems that the rats developed a resistance to leptin's appetite-cutting effects. How to Control Hunger HormonesAre there ways to control our "hunger hormones," and thus rein in our appetites? Possibly -- by avoiding high-fat foods. When we eat, messages go out to various parts of our bodies to tell us we've had enough. But when we eat fatty meals, this system doesn't work as well, says Dallman. Eating fat tends to lead to eating more calories, gaining weight, and storing fat, Dallman says. Researchers have seen some of these effects after only three days of a high-fat diet. But researchers have shown that either a diet rich in either "good" carbohydrates (like whole grains) or a diet high in protein suppresses ghrelin more effectively than a diet high in fat. Something that might help (and certainly won't hurt) is to get enough sleep! In a study of 12 young men, sleep deprivation was associated with an increase in ghrelin levels, appetite, and hunger compared with when they slept 10 hours a night. All in all, this adds to the huge amount of evidence showing that avoiding a high-fat diet is one of the keys to maintaining a healthy weight. Leptin inhibits ghrelin in two ways; it reduces ghrelin secretion by gastric cells, and suppresses the expression of ghrelin receptors in the NPY system, therefore preventing the stimulation of feeding behaviors by the latter. This effect is postulated to constitute the major feedback loop between the organs of eating and the hypothalamus which maintains body weight. When this loop is disrupted at any point, either in terms of timing, duration, or magnitude of feedback impulse signalling, hypothalamic loss of feeding is lost, resulting in obesity. Leptin also increases the rate of thermogenesis and thus promotes weight maintenance. Ghrelin, on the other hand, stimulates feeding and results in obesity. It is produced in the stomach and also in the hypothalamic subparaventricular zone, which has an appetite-stimulant action. Ghrelin levels rises before a meal, and goes down after meals. Related Stories
Experimentally, even when the same type of diet is fed to different rodents, two categories are rapidly formed: the first is obesity-prone and starts to put on weight rapidly, whereas the second group shows a static weight. This can be explained by the fact that the first group alone shows high leptin levels, with low ghrelin levels, possibly caused by the former. Conversely, the other group has no alteration in the secretion of both hormones. Hypothalamic Restraint by LeptinIn another study, leptin lowering was associated with high levels of ghrelin secretion, but there was a centrally-operating suppression of the expected appetite drive despite increased ghrelin. Ghrelin secreted in the stomach mucosa circulates to the brain and crosses the blood-brain-barrier. It acts together with locally secreted ghrelin in the hypothalamus to stimulate the NPY and other neurons in the ARC-PVN nucleus to stimulate appetite. This can be inhibited by Y1 receptor antagonists acting on the NPY neurons. Leptin acts to reduce the synthesis, release, and biological actions of NPY in the ARC-PVN neuronal system via long leptin receptor activation. Yet leptinopenic mice (i.e. those with low levels of leptin) failed to develop a good appetite, though their ghrelin levels rose. Thus the hypothalamic restraint exercised by leptin overrides even a strong peripheral afferent signal by ghrelin. Actions of GhrelinThere are several notable actions that ghrelin has on a human body:
In the anorexic eating disorders, the ghrelin levels are chronically raised, which may be due to the negative state of the body’s energy, and are meant to stimulate the appetite to increase body fat percentage. Nevertheless, it may also mean that such patients are unresponsive to ghrelin. Our gut microbiome is our most important human organ. This complex ecosystem of bacteria, viruses, fungi, archaea, and bacteriophages has been called the conductor of the immune-neuroendocrine system, home of the immune system, and even the second brain. In fact, the gut microbiome’s role in human biology is so widespread that scientists from nearly every specialty are checking for potential health solutions within the gut. With chronic diseases on the rise across the world, the gut microbiome is now front and center in this epidemic.
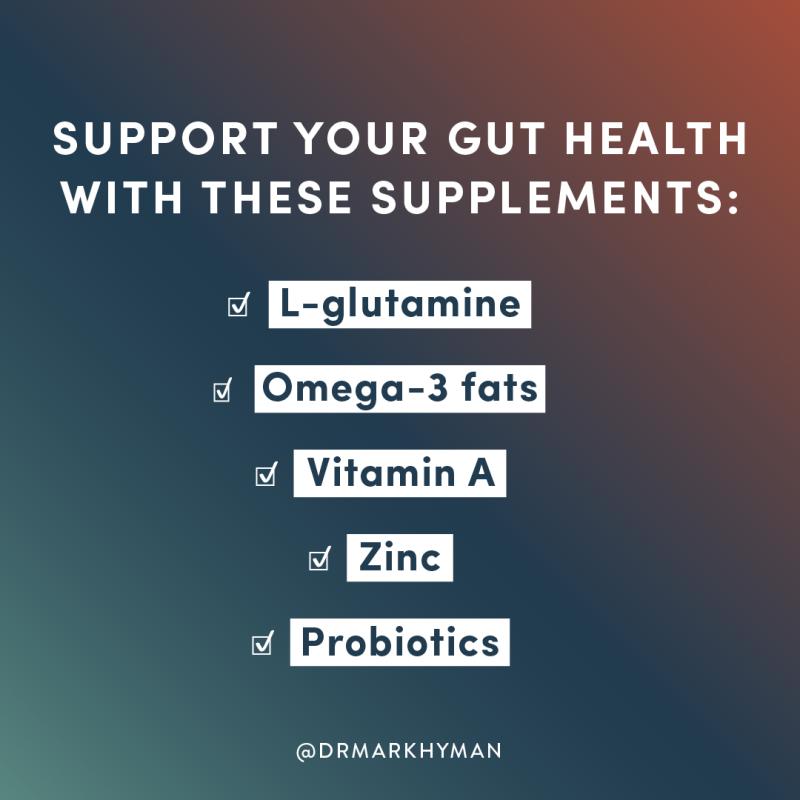
It’s Time To Redefine Our Relationship With Bacteria. Our relationship with bacteria is a complicated one. While most bacteria that live in and on us work in harmony, we only ever seem to hear about bacteria when they cause a devastating outbreak. From the bubonic plague, which is caused by the Yersinia pestis bacteria, to food recalls caused by various Salmonella strains, history is full of occurrences where bacteria have wreaked havoc and caused widespread fear. Even today, antibiotic-resistant bacterial strains like MRSA and CRE (ominously known as “nightmare bacteria”), continue to perplex doctors and researchers. These terrifying scenarios have contributed to the widespread belief that all bacteria are harmful, and fueled our all-out war against microorganisms ever since the discovery of penicillin in 1929. However, mounting research suggests that more often than not, bacteria contribute to our health in positive ways. Scientists now sound the alarm to reexamine our conventional views on bacteria. Not only are these microbes critical to our survival, but they also influence everything from shaping our body to affecting our mood. As Martin J. Blaser, professor of microbiology and director of the Human Microbiome Program at the New York University School of Medicine, put it, “The composition of the microbiome and its activities are involved in most, if not all, of the biological processes that constitute human health and disease.” Why Your Gut Microbiome Matters? Every one of us is covered in microbes with the gut being the richest source. The microorganisms in and on our bodies weigh between two to six pounds, making them heavier than the brain. We each have multiple microbiomes in our eyes, mouth, nose, skin, and if you are a female, also in the vagina. Starting at birth, you are bathed in your mother’s microbiome as you exit her birth canal, which is where you begin building your microbiome. During the first seven years of your life, what you eat and what you come in contact with continues to develop your microbiome. Though your microbiome continues to shift throughout your life, scientists believe that you maintain a microbial signature, or a “fingerprint,” which is most similar to your mother’s. How Your Gut Microbiome Affects Your Digestion? The microorganisms living in your gut help you extract and synthesize many nutrients and byproducts that you wouldn’t otherwise be able to obtain from your food. These microbes: · Digest your food · Create important neurotransmitters · Synthesize vitamins · Produce essential nutrients · Use food to create health-boosting byproducts like short-chain fatty acids We once thought these polysaccharides, oligosaccharides, and other carbohydrates were completely indigestible. But it turns out our microbes break these down and ferment them into beneficial short-chain fatty acids such as butyrate, propionate, and acetate. Short-chain fatty acids help protect against obesity, insulin resistance, and are anti-inflammatory. Due to the disease-fighting power of these fatty acids, Viome’s personalized recommendations aim to support bacteria known to be the highest producers. Our microbes also heavily regulate how much energy we can extract, store, and use from our food. So much so, that scientists believe our weight may have much more to do with what microorganisms are in our guts than how much we eat. How Your Gut Microbiome Affects Your Immune System? The gut microbiome teaches the immune system the difference between friend and foe, making it an integral part of how well immunity functions. In fact, the gut is the home of 70- 80% of our immune system. This interwoven relationship and constant communication between the gut microbiome and the immune system is the primary reason researchers search for cures to all sorts of illnesses by focusing on the gut. An imbalance of gut microbiota, known as dysbiosis, can contribute to an increased weakness of the gut lining, which is more commonly called ‘leaky gut.’ When there are gaps in the gut lining, toxins, bacteria, and food particles can leak into the bloodstream and cause widespread inflammation throughout the body. This process has been implicated in: · Autoimmune conditions · Heart disease · Alzheimer’s · Parkinsons · Allergies · Cancer · Asthma · Obesity · Type 2 diabetes How Your Microbiome Affects Your Hormones? The gut microbiome is so essential in hormonal regulation and balance, it’s now considered part of the endocrine system. Similar to an orchestra playing a harmonious symphony, hormones circulate throughout the body in delicate rhythms, keeping numerous body systems in order. The gut microbiome acts as a conductor for the symphony, making sure everything plays in tune and on time. When your gut microbiome is out of harmony, it can throw off your hormones and cause a variety of health issues ranging from weight gain to thyroid dysfunction. How Your Gut Microbiome Affects Your Mental Health/ Everyone has experienced the feeling of ‘butterflies” in their stomach at some point in their lives. That feeling isn’t merely a sensation, it’s your gut communicating with your brain. The gut-brain connection is constant and even has its designated line of communication, the vagus nerve. In fact, the biggest producer of your happy neurotransmitter, serotonin, isn’t the brain—it’s your gut microbiome, which produces over 90 percent. Changes in the gut microbiome are linked to the mind on many levels including: · Your mood · Your happiness · Your pain tolerance · Your cognitive performance · Your behavior · Your mental health The gut-brain connection is so strong that one of the fastest growing areas of neuroscience looks at the gut first. How Your Gut Microbiome Affects Your Skin? Beauty truly comes from the inside out. The gut microbiome plays a direct role in the appearance of your skin through influencing: · Inflammation—the underlying cause of most diseases · Oxidative stress—a significant cause of inflammation · Tissue lipid levels—an essential factor for a healthy metabolism · Glycemic control—your ability to balance blood sugar · Neuropeptide levels—a factor linked to your mood, pain tolerance, and body’s homeostasis· · Opportunistic bacteria, harmful bacteria that can cause conditions when it overgrows When it comes to autoimmune skin conditions such as eczema, rosacea, and psoriasis, the gut is known to be a major driver behind the worsening of these conditions. The gut’s fundamental role in skin health is why so many creams and lotions are a waste of money. How Your Microbiome Affects Your Heart? Could the gut microbiome be a predictor of heart disease? Researchers from the University of Cambridge seem to think so. They found that specific metabolites, such as trimethylamine N-oxide (TMAO), could be a good indicator of heart disease risk. High levels of TMAO in the body occur when bacteria convert choline into trimethylamine (TMA), which is then absorbed by the body and converted to the harmful version, TMAO. Choline (one of the B-complex vitamins) is found in many animal products and legumes, which might make you want to cut back on these foods. However, the initial part of this conversion from choline to TMA, only occurs when you have certain bacteria in your microbiome. For example, if you have high levels of gammaproteobacteria, which are known for this conversion, it’s more likely that high choline foods are contributing to your heart problems. Everyone knows someone diagnosed with a chronic illness, diabetes, or an autoimmune disease. Moreover, we know that once treatment begins, it can often be too late. Have you ever had a gut feeling or butterflies in your stomach? These sensations emanating from your belly suggest that your brain and gut are connected. What’s more, recent studies show that your brain affects your gut health and your gut may even affect your brain health. The communication system between your gut and brain is called the gut-brain axis.
are on How Are the Gut and Brain Connected? The gut-brain axis is a term for the communication network that connects your gut and brain. These two organs are connected both physically and biochemically in a number of different ways. The Vagus Nerve and the Nervous System Neurons are cells found in your brain and central nervous system that tell your body how to behave. There are approximately 100 billion neurons in the human brain. Interestingly, your gut contains 500 million neurons, which are connected to your brain through nerves in your nervous system. The vagus nerve is one of the biggest nerves connecting your gut and brain. It sends signals in both directions. For example, in animal studies, stress inhibits the signals sent through the vagus nerve and also causes gastrointestinal problems.Similarly, one study in humans found that people with irritable bowel syndrome (IBS) or Crohn’s disease had reduced vagal tone, indicating a reduced function of the vagus nerve. An interesting study in mice found that feeding them a probiotic reduced the amount of stress hormone in their blood. However, when their vagus nerve was cut, the probiotic had no effect. This suggests that the vagus nerve is important in the gut-brain axis and its role in stress. Your gut and brain are also connected through chemicals called neurotransmitters. Neurotransmitters produced in the brain control feelings and emotions. For example, the neurotransmitter serotonin contributes to feelings of happiness and also helps control your body clock. Interestingly, many of these neurotransmitters are also produced by your gut cells and the trillions of microbes living there. A large proportion of serotonin is produced in the gut. Your gut microbes also produce a neurotransmitter called gamma-aminobutyric acid (GABA), which helps control feelings of fear and anxiety. Studies in laboratory mice have shown that certain probiotics can increase the production of GABA and reduce anxiety and depression-like behavior. Gut Microbes Make Other Chemicals That Affect the brain.The trillions of microbes that live in your gut also make other chemicals that affect how your brain works.Your gut microbes produce lots of short-chain fatty acids (SCFA) such as butyrate, propionate and acetate.They make SCFA by digesting fiber. SCFA affect brain function in a number of ways, such as reducing appetite. One study found that consuming propionate can reduce food intake and reduce the activity in the brain related to reward from high-energy food. Another SCFA, butyrate, and the microbes that produce it are also important for forming the barrier between the brain and the blood, which is called the blood-brain barrier. Gut microbes also metabolize bile acids and amino acids to produce other chemicals that affect the brain. Bile acids are chemicals made by the liver that are normally involved in absorbing dietary fats. However, they may also affect the brain. Two studies in mice found that stress and social disorders reduce the production of bile acids by gut bacteria and alter the genes involved in their production. Gut microbes affect Inflammation. Your gut-brain axis is also connected through the immune system. Gut and gut microbes play an important role in your immune system and inflammation by controlling what is passed into the body and what is excreted. If your immune system is switched on for too long, it can lead to inflammation, which is associated with a number of brain disorders like depression and Alzheimer’s disease. Lipopolysaccharide (LPS) is an inflammatory toxin made by certain bacteria. It can cause inflammation if too much of it passes from the gut into the blood. This can happen when the gut barrier becomes leaky, which allows bacteria and LPS to cross over into the blood. Inflammation and high LPS in the blood have been associated with a number of brain disorders including severe depression, dementia and schizophrenia. SUMMARY: Your gut and brain are connected physically through millions of nerves, most importantly the vagus nerve. The gut and its microbes also control inflammation and make many different compounds that can affect brain health. Probiotics, Prebiotics and the Gut-Brain AxisGut bacteria affect brain health, so changing your gut bacteria may improve your brain health. Probiotics are live bacteria that impart health benefits if eaten. However, not all probiotics are the same. Probiotics that affect the brain are often referred to as “psychobiotics”. Some probiotics have been shown to improve symptoms of stress, anxiety and depression. One small study of people with irritable bowel syndrome and mild-to-moderate anxiety or depression found that taking a probiotic called Bifidobacterium longum NCC3001 for six weeks significantly improved symptoms. Prebiotics, which are typically fibers that are fermented by your gut bacteria, may also affect brain health. One study found that taking a prebiotic called galactooligosaccharides for three weeks significantly reduced the amount of stress hormone in the body, called cortisol. SUMMARY: Probiotics that affect the brain are also called psychobiotics. Both probiotics and prebiotics have been shown to reduce levels of anxiety, stress and depression. What Foods Help the Gut-Brain Axis? Health Tip: The Foods Your Brain Craves. A few groups of foods are specifically beneficial for the gut-brain axis. Here are some of the most important ones:
A number of foods such as oily fish, fermented foods and high-fiber foods may help increase the beneficial bacteria in your gut and improve brain health. The gut-brain axis refers to the physical and chemical connections between your gut and brain. Millions of nerves and neurons run between your gut and brain. Neurotransmitters and other chemicals produced in your gut also affect your brain. By altering the types of bacteria in your gut, it may be possible to improve your brain health. Omega-3 fatty acids, fermented foods, probiotics and other polyphenol-rich foods may improve your gut health, which may benefit the gut-brain axis. |
Archives
April 2022
Categories
All
|



 RSS Feed
RSS Feed